Managing Endo and IBS
Interview & article by Jesse Driessen.
Published 18th September 2024.
Gina lives with Endometriosis, IBS and Migraine. In this article, we chat with Gina about how she manages her symptoms, the long journey to find a medical team with the right skills to help her, and the importance of finding a supportive community.
Just to get things started, do you mind just covering quickly the main health conditions that you are managing?
So currently I have a couple of overlapping conditions. I have Endometriosis and IBS, primarily IBS-D. I also get Migraines occasionally. Those are the biggest ones.
I'm not so familiar with the different types of IBS, you mentioned IBSD. What is that?
It’s irritable bowel syndrome. There’s like three different ones that people experience that I know of. So IBS-D is predominantly diarrhoea, so looser stools. IBS-C is predominantly constipation. And then I believe there’s IBS-M, which is mixed. So those are people who have both show up.
How would you say that your health was before you started using Bearable?
I started using Bearable in April of 2022. So at that point, my health was kind of progressing towards being a little bit better in terms of the IBS. I’d been working with a dietitian and gastroenterologist since 2020 when my IBS was at its worst. So, by that time, I’d identified some food intolerances and it was getting a little bit better.
Then last year – in 2023 – is when my Endo got a lot worse and reached this peak. So it’s a little hard to say what my health was like at that point because I was in between the two conditions in a sense. Or at least, figuring out how to manage both conditions.
So when I first started using Bearable, my health was not at its best but it also wasn’t at its worst.
Was the catalyst for looking for an app like Bearable, just that you were suddenly having to manage a new health condition?
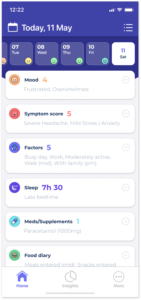
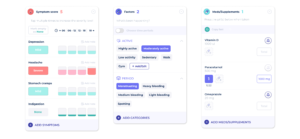
Kind of, but what I remember was that I needed something that was easier for tracking my symptoms. At that point, I was using this really detailed spreadsheet (or my notes app) which was getting really long and hard to use. I also wanted to see correlations.
Because mental health can also be affected by chronic illnesses, I wanted to get an overview of how my mood and energy levels were doing too. Just to see if there was anything that was alarming or anything that stood out in terms of overlapping with my chronic health conditions.
To what extent did Bearable help you to address those needs?
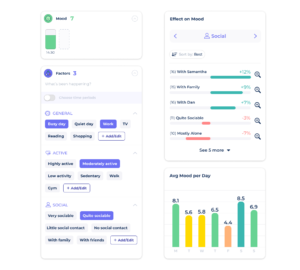
So, Bearable is helpful for me, especially before I go into a doctor’s appointment or a specialist doctor’s appointment. Using the app it’s easier for me to get an overview of, like, how many days per month my symptoms have occurred. Breaking that down by symptom, and also across my overall symptoms, has been helpful for me.
It’s been helpful for me with my mental health and working with my therapist to keep track of my mood each month, like seeing if I have a higher amount of sad days.
Then also, because fatigue does come into play with a lot of chronic health conditions, keeping an eye on my energy levels. Basically it’s helpful for me to get those overviews in order to better prepare for appointments.
Do you mind sharing a bit more about how you're presenting your data from Bearable to your doctor?
So that’s the thing, at least for me, I don’t fully know the best way to export the data. There was one time where I tried to export a month-by-month view of how often I was having my chronic pelvic pain, for example, and I printed that out and I was gonna show it to the doctor. But I noticed it was an overwhelming amount of information.
So I don’t necessarily show them anything from the app. It’s more so that I take the data and condense it for myself, in order to be prepared for an appointment, and tell them what’s going on and what I’m dealing with.
Would you also say that Bearable's had any sort of impact on your quality of life or your well-being more generally as well?
I’m not sure honestly, because I use it for different things. Another app I use is Finch and that one I use more for my mental health, journaling or affirmations. And there’s more of a community connection aspect. You can connect with friends and send them hugs and things like that.
So with Bearable, the perspective I get from the app, or at least my use of it, it feels more introspective overall. Meaning I use it for inputting data and noticing trends and seeing how I’m feeling.
In the beginning, I did use the gratitude feature more often. Like I would write something down every day, but I just got out of the habit of that the past year. Finding the right balance with Bearable was important for me because there are so many options of things you can track. I do appreciate the variety of things you can do, but sometimes it’s a lot of information.
So I wouldn’t say I’ve noticed a direct impact on my mental health. However, if I’m thinking about it, being able to find an easier way to track things has helped my mental health in that it helped offload some of the time and energy it takes to track my health conditions and symptoms.
Like compared to if I used a less user-friendly tracker, like a spreadsheet or a notes app. So I think it does take off some of that mental load and effort and makes it easier to track things.
Would you say that more than helping your mental health and well-being, Bearable is just giving you a clearer picture of your health?
Yeah, I think it definitely does. I think that is honestly the thing it helps me with the most.
Do you mind giving me a quick overview of what your day-to-day experience is with Endometriosis?
Yes, it’s funny to think of a day-to-day experience because it varies so much.
I think my experience might be a little different than what people assume Endometriosis is because most people – when they first learn about it – assume it’s just painful periods. Whereas for me that is how it started but, currently, I’m on a very high progesterone birth control and so I haven’t had a period in over a year and a half. But I still have chronic, recurring pelvic pain due to my Endo.
I think what’s hard to parse out is that oftentimes people with Endo also have gastro issues and other symptoms. So like my IBS very well could be related to my Endo – I just don’t know for sure. But in terms of day-to-day experience, sorry, I don’t really know how to answer that.
I guess a better way to phrase that question might be, what are the things that you think that somebody should know about life with Endometriosis?
Oh, okay, that’s a very big question. So the biggest symptom I experience is chronic and recurring pelvic pain. Sometimes that includes painful bowel movements, sometimes it doesn’t. So generally with Endo, I’m trying to manage it as best I can in terms of reducing how often the pain occurs. Including reducing the intensity of the pain, but also having to accept that it’s chronic so it’s never going to fully go away.
Learning how to live with that pain and manage it better includes treating it in the moment, like with a heating pad or other types of tools. Also how to deal with that mentally, like the grief – there’s a lot of grief that accompanies living with Endometriosis because the way my body shows up and what it can handle has very much changed over time.
Learning to accept that I might not be able to do higher-intensity exercises or might not be able to do sports that I used to enjoy – things like that. Because with Endo there’s a lot of pain but also fatigue. Your body is dealing with high inflammation and then sometimes it also feels like your body is fighting itself. So there’s a lot of fatigue that shows up with Endo and IBS.
"There’s a lot of grief that accompanies living with Endometriosis because the way my body shows up and what it can handle has very much changed"
I think you've touched on a really interesting point. Ultimately, there's a transitional period when you begin living with a chronic health condition. You realise that you're probably not going to be able to do a lot of the things that you used to. It sounds like almost that's kind of an ongoing experience for you?
Yeah. I think, like you said, it feels like I’m going through phases that accompany my chronic health conditions. I definitely felt like the first couple of years, when I found out I might have Endo, it was very much just going online, talking to people, and learning what that even means or what could happen.
It seems like the list of symptoms is endless or there’s always new ones popping up that you didn’t even know about. Like, ‘Oh, that is Endometriosis too?’ It’s like a discovery period of figuring out what that looks like, and trying to see specialists to get a diagnosis or at least get more answers.
Then I would say with chronic conditions – especially Endo and IBS – unfortunately, a lot of it is trial and error. With management techniques like medications or physical therapy, whether or not they help you varies so much depending on the person.
I’m still in a phase where I’m literally just trying different things and seeing if they help or don’t help. That phase can be pretty exhausting because you’re trying new things over and over again. Sometimes the side effects are really bad and you’re like, ‘Okay, that’s not for me.’
Then I think after that it’s just management. Learning how to live with it and manage it the best you can. But the hard thing with Endometriosis is that even if people have excision surgery (the laparoscopic minimally invasive surgery) and you get it removed, it can grow back, which I feel might be unique for a chronic condition.
There’s a lot of fear and uncertainty about whether it will change, if it will grow back, and if it will get worse. Trying to accept that, taking things day by day, or trying to accept that this is how it is for me in this moment can help. Like I can only control what I control.
Were there any specific tools you use to help you to come to terms with living with these conditions?
There’s a few that might feel obvious but I think are still important to name. Talk therapy is what I started with.
I was finding that there were times when a flare-up would happen and it would feel like it’s never going to end. So it can kind of feel like: ‘What if it gets worse? What if it doesn’t end? What if it disrupts my work?’ That can be really scary and the emotions can be overwhelming in the moment.
My therapist suggested utilizing some DBT techniques (dialectical behaviour therapy) and I feel like that is helpful in separating your emotions or feelings from fact. Also, for trying to learn to let your emotions come in waves and accept them. Like just letting them pass by so that you’re not internalizing it all as much. It’s not always perfect, but I think those are the biggest tools for me.
I think one of the silver linings of having chronic conditions like Endometriosis is that you learn out of necessity to get better with boundaries. Like being vocal when you might need to take a break, rest during a trip, or say no to plans. Because if you overdo it or if you plan too much, then your body will feel it the next day.
You've mentioned how your main symptoms are essentially forms of pain and that they can be quite unpredictable as well. Does that have a big impact on your ability to plan certain activities e.g. socialise or work?
It does to a certain extent. For the first time in my life, this past year, I’ve been able to request accommodations at work. That has been helpful, but it’s one of those things where I’m lucky that my boss is very understanding. I know if your supervisor isn’t supportive, that can put you in a really bad spot.
For social plans, I’m lucky to have friends who have a shared understanding that if you need to cancel or reschedule, that’s okay. I don’t necessarily have any in-person friends that also have Endometriosis. However, I have friends who have varying degrees of depression, anxiety, or other health conditions. So there will be times when they need to cancel or reschedule and that means it’s okay if I do as well.
I’ve also gone on some trips with my mom. For example, we went to a state fair and we were gonna go see this musician. Then before the show, I started having some pain and I needed to sit down. So we adjusted our plan for a moment. We just sat on a bench, got a funnel cake or something, and people watched and waited it out.
We still made it to the show and it ended up being fine. So having people who are supportive or understanding – even if they don’t understand the condition – just that you might need to adjust plans really helps.
For work, unfortunately, there are certain jobs I would not be able to do and that wouldn’t be feasible for me. Any job where you’re on your feet all day or have to do a lot of manual labor, for example. So I have a desk job, but I still need accommodations for the days I have to go into the office.
Do you mind also telling me a little bit about your day-to-day experience with IBS as well?
Yeah, that one’s actually a little easier for me to succinctly describe. But it’s also very unpredictable as to when it shows up.
I’ve identified some food intolerances and so I avoid those and it got a little better. But a lot of people say ‘Oh, just don’t be stressed’ or ‘Get more sleep’. Even if I do those things, my IBS is still showing up.
Most days, my IBS isn’t an issue but then at least once a week it is. Sometimes more, depending on the month. Basically, the way IBS shows up in my life is it’ll just disrupt it inconveniently. Sometimes I’m working at home, so it’s not as bad to deal with. However, sometimes if I’m at work or on a trip, I don’t want to be too graphic, but I need to be near a bathroom.
For me, the way I somewhat manage my IBS is by avoiding certain foods. I also have prescription antispasmodics which basically slow your gut and calm it down. Those do help and I can take them preemptively if I’m worried about a certain workday or trip.
However, one of them really dries me out. It gives me a headache and sometimes a migraine if I don’t drink extra water. So I don’t love taking that, but it’s my best line of defence currently. You also have to be careful not to take antispasmodics too often, because I was told by my gastroenterologist that they can be less effective if you do.
Basically, the way IBS-D shows up is that it just disrupts your day at inconvenient times and you just have to deal with it because you have no other choice.
You’ve already mentioned that - to some degree - IBS might be related to Endometriosis. Are there any ways they influence each other in terms of your overall health?
I’m still figuring it out because when I do have an IBS flare up I often have pelvic pain or pain that comes on right before it happens. So I don’t really have a lot of notice, and I’m not sure if it’s related to the Endo or not. Because on the flip side, I have plenty of Endo pelvic pain flare-ups where I don’t have an IBS issue.
Generally, in terms of those things happening or working together, that can lead to more fatigue and it tires you out. It’s a lot wear and tear on your body. That’s when sometimes the mental health comes into play too, where you just feel like ‘this really sucks,’ ‘this is hard and overwhelming,’ and I don’t want to deal with it.
That's when sometimes the mental health comes into play too, where you just feel like ‘this really sucks,’ ‘this is hard and overwhelming,’ and I don't want to deal with it.
Are there any things you're doing that seem to help with both conditions?
Not necessarily.
It really varies depending on the person, so it’s more trial and error. Trying different things and seeing if it helps with lowering the amount of flare-ups per month. I started a medication called gabapentin when my pain was at its worst, and that seems to help both my Endo and IBS to an extent. But then I got COVID earlier this year and my IBS got worse again, so things can always change.
In general, I’ve made sure not to over-schedule or over-commit myself. I noticed one weekend when I did that, it got really bad. The basic recommendations of getting enough sleep, eating enough, and managing stress do help inadvertently.
One thing I did try recently is gut-directed hypnotherapy. You can do it with a specialist or in person, but I just use an app. Basically it’s hypnotherapy that is more focused on the gut, but it also acts as a nice, relaxing meditation too. So I try to do that every morning.
Another thing that helps is resting when I need to. I do notice that – because of brain fog – I’ll reach a point each day where I need to mentally and physically take a break.
So part of my workplace accommodation is having a private space to do a meditation (sitting or lying down) and closing my eyes for like 10 minutes. I noticed that helps with my energy levels.
It’s hard because with Endo pain and IBS it’s a delicate balance of not overdoing it with your body. But some form of movement is helpful because otherwise, my fatigue can get bad. So gentle movement like taking walks or low-intensity movement, in general, helps both my Endo and IBS.
I’m in the process of trying acupuncture to see if that helps, but it’s too soon to know yet.
What's the name of the app that you use for the gut-focused hypnotherapy?
Years ago, I tried one that my dietitian recommended called Nerva. However, it’s really expensive. I recently found one that’s run by this woman, Jayne Corner, called the Calm and Happy Gut app and it’s more financially feasible for me. There’s also some CBT exercises in the app and they’re helpful for managing your emotions or thoughts.
How’s Bearable helping you to manage Endometriosis and IBS?
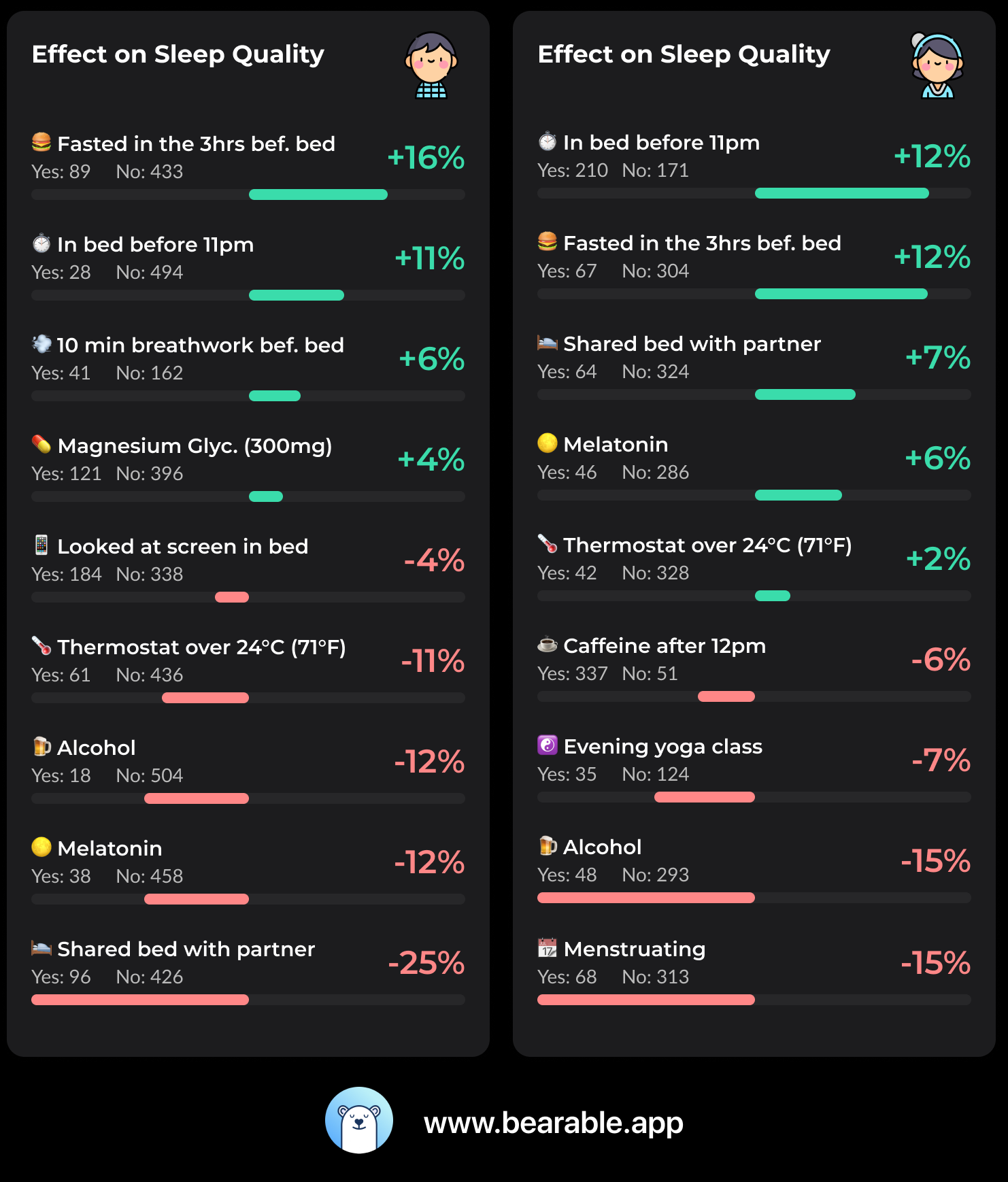
I think it helped me differently when I first started using it, versus now when I have a better idea of my health conditions. In the beginning, I think it was helpful to see if there were any correlations. For example, if I did more exercise than usual, was I more likely to have days of IBS issues?
Seeing things like that was more helpful in the beginning. Compared to now, I have a better idea of the general things that seem to help or hurt me. So I don’t really use that as often.
For me now, I’d say it’s more helpful for making it easy to track things and – at a glance – see how things are going. For my own reference and also to prepare for medical appointments and things like that.
Do you have any other recommendations or resources that you want other people living with these Endo and IBS to know about?
It’s a little hard to find, but there are a few free Endo and pelvic pain support groups that exist that I found really helpful. If you search within Facebook groups or Reddit, r/endo or r/endometriosis, those can be really helpful. Especially if you have a new symptom showing up and you’re wondering if anyone else experienced the same thing. It can be helpful in advocating for yourself at the doctor’s office.
It’s hard because, from what I’ve been told about chronic pain, it’s like these neural pathways that have been established. Even with IBS, my dietitian has described that it’s like a hypersensitivity in a sense. So sometimes if I’m worried about my pain, or worried about my IBS flaring up, it can show up differently. Or I can have pain move to a different part of my body. That’s when I’m like ‘Oh no, is this something new that I should be concerned about?’ So in those moments, the support groups can be really helpful in feeling less alone. And if a new symptom lasts, then I’ll mention it to my doctor.
There’s one virtual, monthly pelvic pain support group that is through an app called Lasa Health, which was co-founded by a woman who also has chronic pelvic pain, Margaret Melville.
There’s also a therapist, Casey Berna, who has a monthly, virtual Endo support group and I found those to be really helpful.
Finding a good specialist for Endometriosis or IBS – which would be a gastroenterologist – can be hard sometimes. But if you can, like those are helpful.
I found a good pelvic pain and Endo specialist who has been really helpful for guiding me through the different things I can consider to try. Whether it’s medications, birth control, surgery, or alternative treatments like acupuncture.
Pelvic floor physical therapy is something that can be really helpful for some people and was somewhat helpful for me. There’s just so many options, honestly. So I think if you’re feeling overwhelmed, a good place to start is with a doctor you trust and gathering data from support groups to learn more about Endo and IBS.
We often hear that people struggle to find a good doctor. But have you had a fairly positive experience with your medical team?
So, oh boy. For the most part, I haven’t had good experiences, but now I have some that are good.
It’s really a journey, which can be frustrating. The average time for someone with Endo to even get a diagnosis is around eight years. For me, it was about three or four years. I got lucky with my primary care physician. They’ve always been someone who’s been very good at listening and validating my experiences.
With IBS, my experience and what I’ve heard from others is that it’s hard to find a good gastroenterologist. I’m actually about to see a third one later this year and I’m more hopeful that they will be helpful because I have friends and coworkers who have had positive experiences with that specific clinic.
With the first gastro’ I went to, she did try some things, but she didn’t really listen to me or communicate to me what fully she considered or tested me for. There was a time when she basically said, ‘I don’t think I can help you anymore, but you should get an MRI because you might have Endometriosis’. So I’m grateful for that at least.
Earlier this year, I saw a second gastroenterologist – who I waited six months to see. It’s sometimes hard with specialists, especially seeing a new one, because you’re condensing years of experience into a five-minute description. When I did that, he basically said that it sounded like my quality of life was good enough and that I should be fine. That was a pretty invalidating and not a great experience. That obviously led me to seeking out a third gastroenterologist.
I think another thing with chronic health conditions, which is beyond the question you asked, but that could be helpful for others is: don’t be afraid to seek a second opinion. With my Endo, the first OBGYN I saw was very kind, but she didn’t know enough about Endometriosis.
She put me on birth control which had the highest amount of estrogen. Which, with Endo, you don’t want because, ideally, you’re trying to reduce the estrogen. So that led to the worst pelvic pain of my life so far. I was in so much pain and she wasn’t giving me options for pain management.
That led me to seek another OBGYN. The second OBGYN was fantastic, knew a lot more about Endo, and took the time to listen and help me. That led to the referral for the pelvic pain and Endo specialist that I see now. So I would say generally my experience with doctors has been mostly negative but – after years – I’ve found some that are helpful. I’m still searching for the right gastroenterologist.
"I think another thing with chronic health conditions... that could be helpful for others is: don’t be afraid to seek a second opinion. "
Why do you think it’s so hard to find good Endo and IBS specialists?
Part of the reason Endometriosis is harder to diagnose is that, technically, it can only be officially diagnosed through laparoscopy (a minimally invasive surgery). It’s ridiculous that you need a surgery to diagnose it. I just got “lucky” that you could see some of it on an pelvic MRI.
Then with IBS, there’s no test for that either. It’s basically a diagnosis of exclusion, ruling out ulcerative colitis, IBD, and other things like that. Just making sure you meet certain criteria of frequency. But other than that, there’s no test for it.
I think that’s part of the reason it makes it hard to find a doctor who can really help. Also, because there’s no cure and the management techniques vary by person, it seems like the doctors are also kind of doing trial and error in a sense.
Do you have any recommendations for how to prep for a medical appointment with Bearable?
For me, the best way to prepare is by writing things down.
Basically, I’ll write down questions I want to ask and summarize what’s in Bearable and put it into a document. For example, how often my symptoms have shown up since I last saw my doctor.
It helps me to be a better advocate for myself in the appointment. Since a lot of times, I’ll go into the appointment and I’ll either be nervous or can’t think of the question I want to ask when I’m on the spot.
You mentioned that you're using support groups. It sounds as though that's quite a big part of your management process.
Yeah, I think it’s really helpful because sometimes you need that specific kind of support. Other people in my life can sympathize and be kind, but they can’t fully understand.
The reverse of that, is it also feels good to help others in the support groups too. Like hopefully accelerating the discovery process for them, or offering options of management techniques they can discuss with their doctor. That can feel very rewarding.
For me, having a purpose can be really helpful for dealing with chronic health conditions. Sometimes when you are in so much pain, you need something to keep you motivated or pull you out of the overwhelming feelings that come up. So I think that’s an important thing too.
Note. The names and information in this article have been used with the permission of the interviewee.

Veronica | Headaches, Lymphedema, and Depression
How I manage Lymphedema, Headaches, Anxiety, and Depression Interview & article by Jesse Driessen.Published 23rd July 2024. Veronica lives with Lymphedema, Headaches, Insomnia, Anxiety, and Depression.

Jennifer | Migraines, ADHD, MCAS, Ehlers-Danlos syndrome, Anxiety, Depression, and Intestinal tract issues.
How I manage ADHD, MCAS, and EDS Interview & article by Jesse Driessen.Published 29th May 2024. Jennifer lives with ADHD, Mast Cell Activation Syndrome (MCAS),

Laura | Long Covid
How Laura uses Bearable to manage Long Covid. I started using Bearable because I have had long covid for two years now. In the beginning







 My goal in seeking an app was to track my illness and my day-to-day. I wanted *one* app that would log my symptoms, moods, and daily life, a place that would allow me to take notes on what happened that day. My memory isn’t great, and if I didn’t know what happened, I didn’t know how I could work to make it better. What was this mood? What were my symptoms at the time? What triggered it? Did I have to take medication to treat it? I knew none of the answers, let alone be able to communicate them to my doctors.
Therefore, the biggest benefit to
My goal in seeking an app was to track my illness and my day-to-day. I wanted *one* app that would log my symptoms, moods, and daily life, a place that would allow me to take notes on what happened that day. My memory isn’t great, and if I didn’t know what happened, I didn’t know how I could work to make it better. What was this mood? What were my symptoms at the time? What triggered it? Did I have to take medication to treat it? I knew none of the answers, let alone be able to communicate them to my doctors.
Therefore, the biggest benefit to 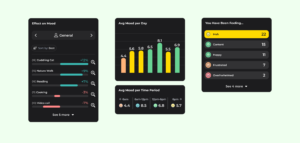 Bearable has literally become a lifeline for me, and I imagine it would be for others, too. Not all patterns are obvious to someone with schizophrenia or bipolar disorder, and it’s amazing to have one organized place to learn about yourself. I can tell my doctors when I’m having a bad week and what important event might have triggered that. I can tell when my medications are working and how often I take them. I have insight into myself, and that would be invaluable for anyone with schizophrenia, bipolar disorder, or any illness at all.
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
Start to reclaim control over your well-being today! Download Bearable for free on
Bearable has literally become a lifeline for me, and I imagine it would be for others, too. Not all patterns are obvious to someone with schizophrenia or bipolar disorder, and it’s amazing to have one organized place to learn about yourself. I can tell my doctors when I’m having a bad week and what important event might have triggered that. I can tell when my medications are working and how often I take them. I have insight into myself, and that would be invaluable for anyone with schizophrenia, bipolar disorder, or any illness at all.
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
Start to reclaim control over your well-being today! Download Bearable for free on 

 So I started the hunt for an app. I wanted to track my cycle – but I didn’t want pink and flowers, I didn’t want reminders of my fertility (getting pregnant is not the only reason we might want to keep track!). I just wanted a calendar that showed the phases as I entered them! I was forgetting my meds constantly too… (I remember taking them… but was that just before…? Or was that yesterday…) So I figured, an app to remind me would be great! Even better if it does both those things! But every medication app in existence wanted me to go count how many pills I had so it could monitor my supply… and cycle apps didn’t care if I was on medication or not.
I searched high and low for this magical app. I didn’t think I was asking for that much – just an app that could keep track of my meds, remind me to take them – that could put a little marker on some days of the month for me – maybe that I could look at a little graph of my weight fluctuations? Or that I could graph my mood maybe!
So I started the hunt for an app. I wanted to track my cycle – but I didn’t want pink and flowers, I didn’t want reminders of my fertility (getting pregnant is not the only reason we might want to keep track!). I just wanted a calendar that showed the phases as I entered them! I was forgetting my meds constantly too… (I remember taking them… but was that just before…? Or was that yesterday…) So I figured, an app to remind me would be great! Even better if it does both those things! But every medication app in existence wanted me to go count how many pills I had so it could monitor my supply… and cycle apps didn’t care if I was on medication or not.
I searched high and low for this magical app. I didn’t think I was asking for that much – just an app that could keep track of my meds, remind me to take them – that could put a little marker on some days of the month for me – maybe that I could look at a little graph of my weight fluctuations? Or that I could graph my mood maybe!
 Every day, three times a day, the little bear pops up to say hey, medicine time! I take my meds, open the app to mark them as taken – and hey, while I’m here, I might as well check in! How am I feeling? What’s going on with my day? Any symptoms? Bam! Less than 3 minutes, done and dusted and all in one place.
First thing every morning I stick my temperature, weight, that sort of thing into my Health app – Bearable grabs it for me! My Watch keeps track of my heart rate (gotta make sure those stimulants aren’t pumping me too far up!) – Bearable grabs that too!
Since using Bearable, I’ve been able to track patterns – I now know when I’ll need more ADHD meds because the hormones make them less effective. No more wondering why everything sucks three days in…
I now know that I actually only need half the antidepressants I used to be on – woohoo!! ! With depression, a bad day feels like forever – now, I can look at the little calendar and see, it’s only been two days and this happened last time we had to go to the dentist too, it’ll pass! (I had never even considered tracking stuff like appointments, when I see family and friends, or factors that could affect my symptoms before! And I called myself a scientist??)
This app is seriously my hero. If you have ADHD or depression, if you’re trialing medication and tracking side effects, or even if you just want a straight-forward way to track your moods during your cycle – this is the one. You have found it!
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
Start to reclaim control over your well-being today! Download Bearable for free on
Every day, three times a day, the little bear pops up to say hey, medicine time! I take my meds, open the app to mark them as taken – and hey, while I’m here, I might as well check in! How am I feeling? What’s going on with my day? Any symptoms? Bam! Less than 3 minutes, done and dusted and all in one place.
First thing every morning I stick my temperature, weight, that sort of thing into my Health app – Bearable grabs it for me! My Watch keeps track of my heart rate (gotta make sure those stimulants aren’t pumping me too far up!) – Bearable grabs that too!
Since using Bearable, I’ve been able to track patterns – I now know when I’ll need more ADHD meds because the hormones make them less effective. No more wondering why everything sucks three days in…
I now know that I actually only need half the antidepressants I used to be on – woohoo!! ! With depression, a bad day feels like forever – now, I can look at the little calendar and see, it’s only been two days and this happened last time we had to go to the dentist too, it’ll pass! (I had never even considered tracking stuff like appointments, when I see family and friends, or factors that could affect my symptoms before! And I called myself a scientist??)
This app is seriously my hero. If you have ADHD or depression, if you’re trialing medication and tracking side effects, or even if you just want a straight-forward way to track your moods during your cycle – this is the one. You have found it!
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
Start to reclaim control over your well-being today! Download Bearable for free on