Taking a cold shower falls into the unique category of things that I recommend trying despite absolutely despising them. Other things in this category include public speaking, running for charity, and eating maatjesharing.
Like these things, cold showers were – spoiler alert – definitely good for me. But why did I decide to torture myself in an attempt to improve my health and where did this practice even come from?







Why do you keep hearing about cold showers?
Despite winter swimming and ice baths being traditions in Scandinavia and Russia. Interest in the health benefits of cold showers has been on the rise over the last 15 years in the rest of the world. In fact, you’ve almost certainly come across the name Wim Hof. Especially if you have an interest in personal development, growth hacking or self-care. The Dutch extreme athlete and Iceman markets a method that involves; cold therapy, breathing, and meditation. To “reduce stress”, “increase willpower”, and “boost alertness” amongst other things. Because of this, when I think of cold showers I think of the 5am club, Soylent and Tech Bros. People who will attempt to squeeze one last drop of efficiency out of every moment in life. Wim made waves in Silicon Valley in 2017, where Cryo-chambers and cold showers have since become a hot trend.Are cold showers good for your health?
The benefits reported from a number of clinical trials and other research show that they can:- Relieve the symptoms of Depression
- Help to prevent sickness
- Improve metabolism and circulation
- Increase the release of Endorphins

Why I decided to start taking cold showers.
Honestly, I’m a warm person. I wear sweaters in summer. I take showers at the hottest setting. I hate being cold. Ultimately this is why I hadn’t jumped on the cold shower train sooner. I didn’t have high hopes that it would be something that I could easily endure… I also wondered if perhaps I wasn’t truly Dutch enough. However, as someone that lives with Anxiety, Depression, and Insomnia (amongst other things). It’s hard to ignore the amount of compelling – even if sometimes anecdotal – evidence that cold hydrotherapy might help with at least one of these chronic conditions. Since cutting out caffeine, I also struggle with a mid-afternoon dip in energy and focus. I hoped cold showers might help with this too.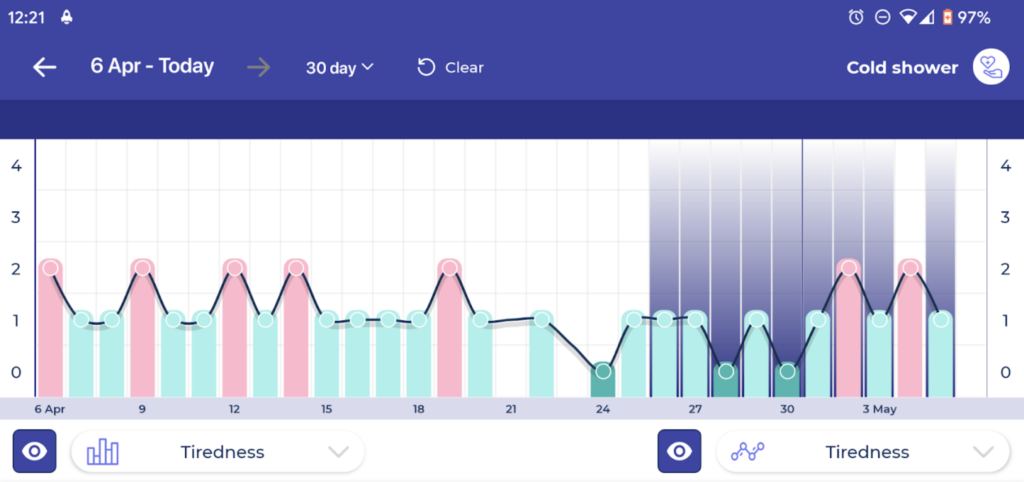
How do you take a cold shower?
You just climb in a cold shower right? I mean, you can do that, and it probably works better than other methods because of the pure shock of the experience. At least according to the cold showers subreddit. It probably also helps if you live alone because you’ll almost certainly hyperventilate, swear, and shout a lot more than if you ease yourself into it. Having researched the best approach for newbies on Reddit and wimhofmethod.com, I took the following approach:- Start with the shower at normal temperature.
- Slowly, step-by-step, turn the temperature down
- When the water is no longer bearable set a timer for three to five minutes
- Practice deep breathing to distract yourself from the cold/torture to help with hyperventilating
- Try to be mindful and focus on being present in the water
- Turn off the shower and feel a sense of accomplishment
Taking cold showers for seven days straight.
Day One: I felt energised and alert, though I had also slept better than usual the night before. The cold shower made me oddly nostalgic but also cold. I felt a bit like I was going to get sick all day. Despite this, I had a productive and focused day with very few symptoms to report. Day Two: I woke up earlier than usual after a good night’s sleep. The cold shower was easier than day one. I felt I had some more energy than normal. I also felt I was more tired and less alert than on day one. Day Three: I slept really well and woke up feeling well-rested for once. After the shower, I mostly felt cold and a bit run down but also alert and in control. Day Four: I had a bad night of sleep but after a cold shower I felt awake and had no tiredness. My mood improved throughout the day and I felt clear and alert. I also fell asleep easily that night. Day Five: I had another good night of sleep. I woke up and dreaded the shower. I forced myself to do it and felt good for not giving up. I had a lot of energy and did a longer dog walk than normal. My mood was good. Stress and Anxiety from work piled up during the day but I was able to remain alert and objective. Day Six: Saturday. I was worried that I’d struggle to commit to the cold shower when it wasn’t part of my morning routine. I also wondered if it would be harder to notice the effects outside of a work environment (where my anxiety tends to be worse). I ended up enjoying it more as it was a warm day and the cold shower made me want to spend the day moving my body. I went for a long hike. Day Seven: I was reluctant to take the last shower. It was a cold, lazy Sunday. I didn’t need to feel alert, or awake. I took the shower anyway. I didn’t regret taking it but I also hated it more than any of the other days. I had a productive day of writing, editing, and photography.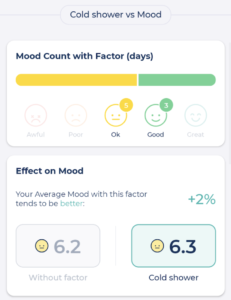
What did the data in Bearable show me?
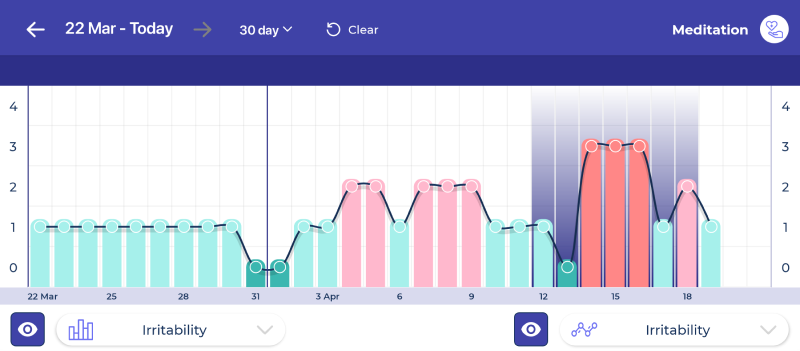
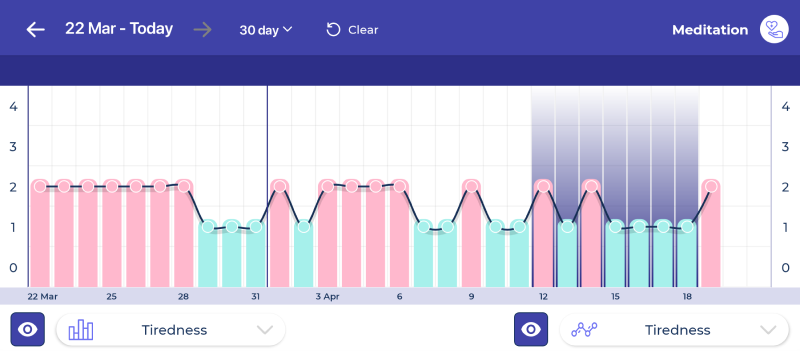
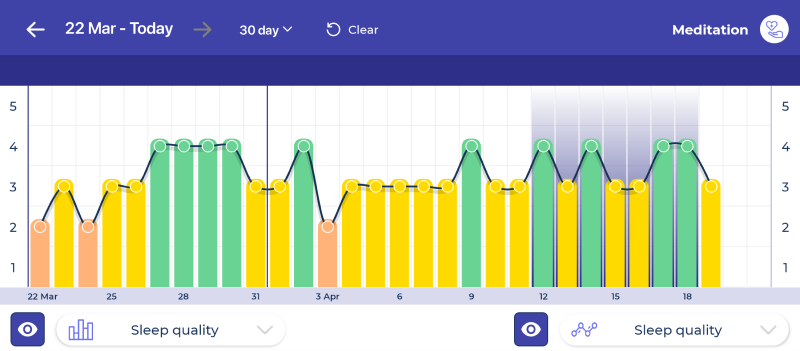
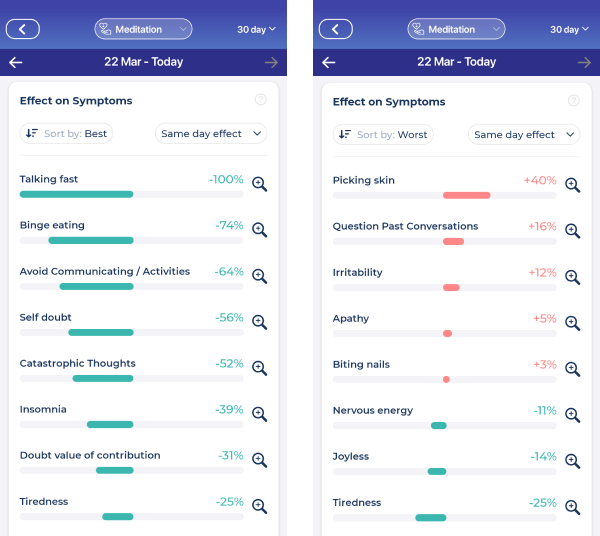
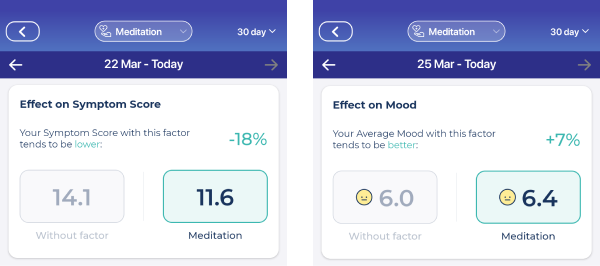
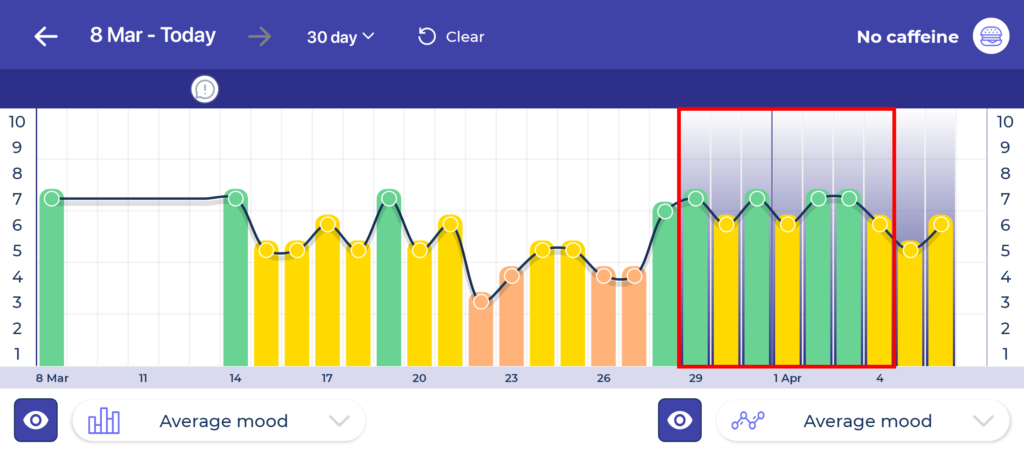
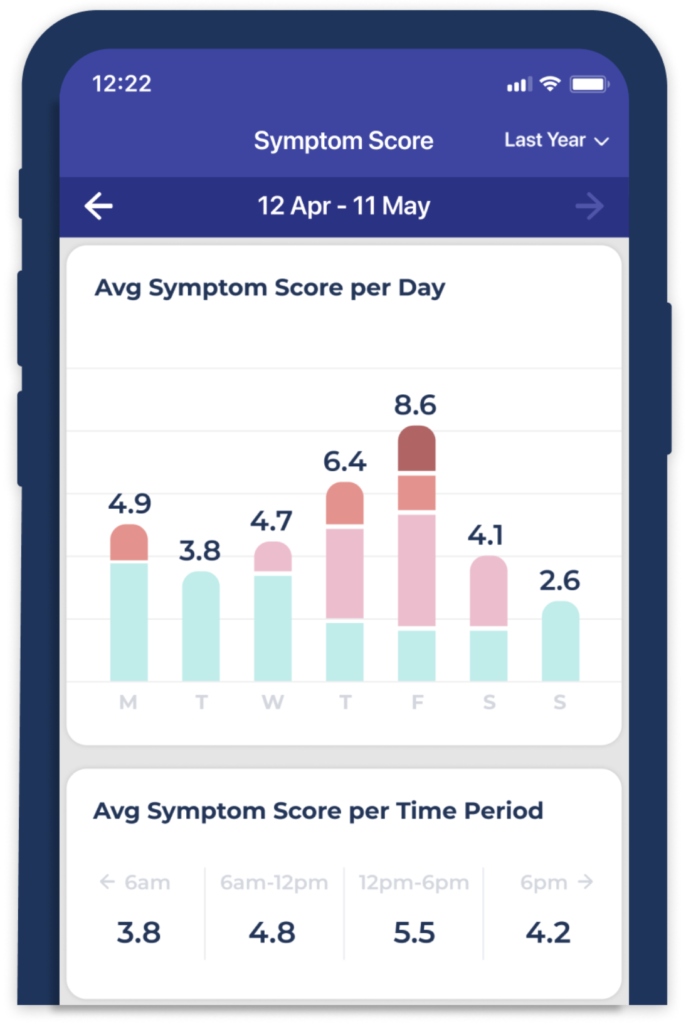
My average Mood improved by just 2% and My average Symptom Score improved by 48% My average Sleep Quality declined by 5% and my average Sleep Quantity declined by 2% My Energy levels declined by 1%The effects on specific symptoms were:
- Irritability improved by 68%
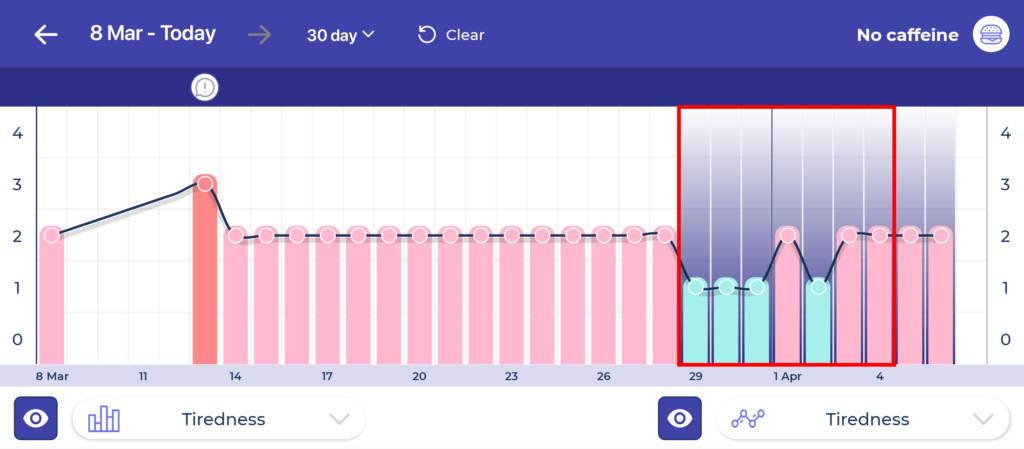
- Tiredness improved by 42%
- Doubting value of contribution improved by 47%
- Self Doubt improved by 29%
- Avoiding social situations improved by 29%
- Catastrophic thoughts improved by 55%
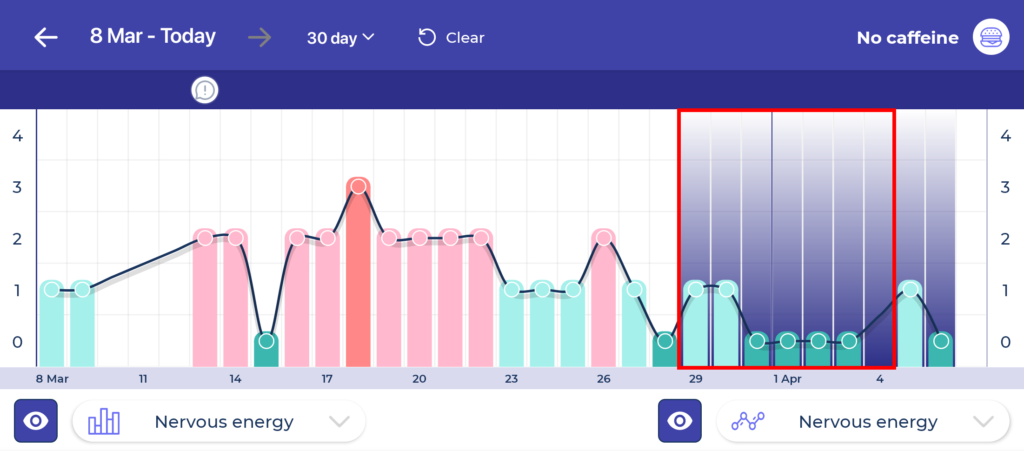
- Nervous Energy improved by 72%
- Apathy was unaffected with 0% change
- Joylessness was unaffected with 0% change
How did cold showers affect my health?
You can see from the results above that cold showers had very little impact on my Sleep, Mood, or Energy but had a fairly significant effect on my Symptoms. Weirdly, some of these things are a bit contradictory. For example, why did my insomnia improve but not my sleep quality or quantity? This data also seems at odds with how I felt during the week. I had felt like I had more energy, was in a better mood, and slept better!?
So did cold showers have a positive impact or not?
Taking a step back from the data, I think the biggest impact that cold showers had was that they made me feel less tired and more focused and alert. Something I don’t very often feel as a result of Anxiety, Depression, and Insomnia. Essentially, I was able to concentrate better on my work and this had a positive knock-on effect on everything else. More focus gave me a better sense of control over my work and being more alert during conversations made them less overwhelming. Because the symptoms of my anxiety were reduced, I was less likely to have nervous energy or spiral into catastrophic thoughts. This also made me less irritable. Something else that’s harder to see in this data is that the average time I would go to bed was more likely to be 10pm than 12pm. Whilst I still woke through the night and tended to wake up earlier than my alarm, I didn’t struggle to fall asleep as much as usual. This is presumably why I reported less insomnia despite my sleep quality and quantity remaining the same.
What are the Pros and Cons of cold showers?
For me, the pros of cold showers are that they led to me having more focus, being more alert, having fewer flare-ups related to Anxiety, and finding it easier to fall asleep at night. The cons are that it didn’t have a bigger impact on my health. My sleep didn’t improve. My mood didn’t improve. My energy didn’t improve. It’s important to point out that this was just a short test. After 7 days I’m certain that I’ve not experienced the full benefits of cold showers. As a result, I’ll continue to take them, especially on days where I feel I lack concentration, focus and awareness. Or perhaps on days when the symptoms of my anxiety flare-up.“Discipline is doing what you hate to do, but nonetheless doing it like you love it.”During my week of cold showers, I came across this quote and it continues to help me to step into cold showers in the morning. When you decide to take the plunge, hopefully, it can help you too. Good luck! —